November 09, 2023
Adrenal stress, cortisol, and weight management: Exploring scientific pathways and nutritional support
Read Time: 3 Minutes
By: Scientific Team at NeuroScience
Healthy weight management can be difficult for many people. While several factors contribute to weight, a person’s experienced or perceived stress is a primary component.
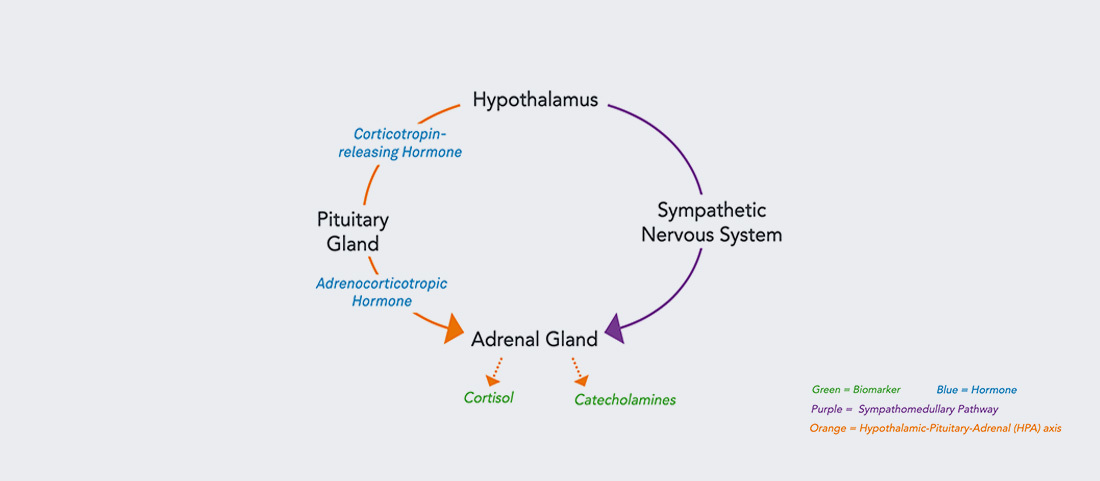
When stressed, the body secretes the hormone cortisol via the hypothalamic-pituitary-adrenal (HPA) axis as part of our normal “fight or flight” stress response. While cortisol has many important neuro-endocrine bodily functions such as impacting a healthy sleep cycle, if unchanged over time, high or elevated cortisol may become problematic in regard to weight management.*
Metabolic effects of cortisol and adipose tissue
Cortisol has been shown to inhibit the release and action of insulin, which can disrupt blood glucose levels (see Figure 1).[1] Blood sugar dysregulation has been associated with weight-related health goals.[2] These connections can become especially important during times like holidays, which favor high stress environments and foods high in sugar.
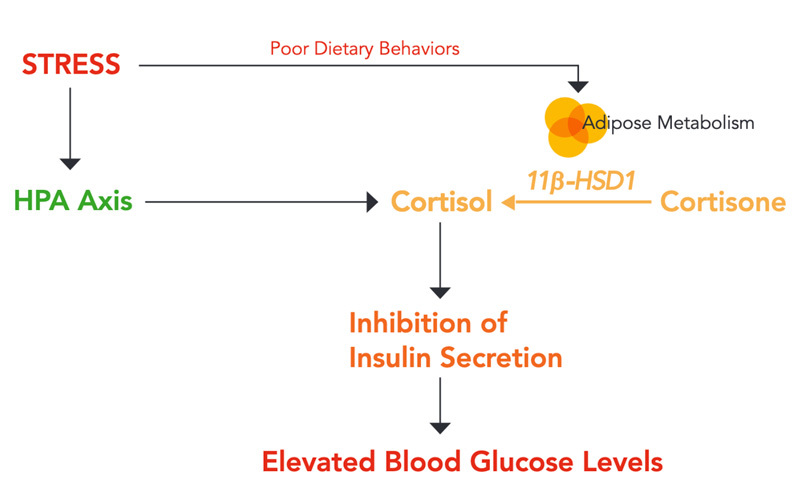
In addition to the impacts on blood sugar levels, cortisol also influences fat metabolism in our bodies (see Figure 1). Cortisol drives an increase in fat deposition by upregulating genes involved in fat storage.[3] Fatty (adipose) tissue further raises cortisol levels by expressing high levels of 11-beta hydroxysteroid dehydrogenase 1 (11β-HSD1), an enzyme that catalyzes the production of cortisol from its inactive form of cortisone.[4]
Nutritionally supporting healthy stress responses
Corosolic acid, a botanical extract found in various plant species like the Banaba tree (Lagerstroemia speciosa), has been shown to support lowering blood sugar levels.[5]* Interestingly, corosolic acid not only promotes healthy blood sugar levels, but also plays a role in reducing cortisol production by inhibiting the 11β-HSD1 enzyme.[6]*
Phosphatidylserine (PS) is another substance that has been widely studied for its impact on HPA axis output.* Ubiquitously found in our bodies as a component of cell membranes, exogenous PS has shown an ability to dampen the cortisol response to both physical and mental stress.[7,8]*
While corosolic acid and PS may have direct effects on our cortisol output, there are also indirect options.* Taurine is an amino acid and potent antioxidant that has shown GABAA receptor agonist properties.[9]* GABA is the dominant inhibitory neurotransmitter in the brain and regulates the HPA axis.[10] Additionally, glycine is an inhibitory neurotransmitter that calms the brain and helps promote sleep.[11]*
Connecting to healthy weight management
Stress, cortisol, and fat certainly have an intimate and influential relationship with one another. This may be why addressing just one component (like diet alone) may not produce desired health goal outcomes. Effectively managing stress, understanding how cortisol works, and promoting positive dietary behaviors can all contribute toward healthy weight management.*
Interested in learning more about stress? Read how the body communicates when its stress tolerance is challenged >
References:
- Schernthaner-Reiter MH, Wolf P, Vila G, Luger A. Front Endocrinol (Lausanne). 2021;12:626427.
- Martyn JA, Kaneki M, Yasuhara S. 2008;109(1):137-148.
- Lee MJ, Pramyothin P, Karastergiou K, Fried SK. Biochim Biophys Acta. 2014;1842(3):473-481.
- Chapman K, Holmes M, Seckl J. Physiol Rev. 2013;93(3):1139-1206.
- Miura T, Takagi S, Ishida T. Evid Based Complement Alternat Med. 2012;2012:871495.
- Rollinger JM, Kratschmar DV, Schuster D, et al. Bioorg Med Chem. 2010;18(4):1507-1515.
- Hellhammer J, Fries E, Buss C, et al. Stress. 2004;7(2):119-126.
- Starks MA, Starks SL, Kingsley M, Purpura M, Jäger R. J Int Soc Sports Nutr. 2008;5:11. Published 2008 Jul 28.
- Schaffer S, Kim HW. Biomol Ther (Seoul). 2018;26(3):225-241.
- Camille Melón L, Maguire J. J Steroid Biochem Mol Biol. 2016;160:196-203.
- Kawai N, Sakai N, Okuro M, et al. Neuropsychopharmacology. 2015;40(6):1405-1416.
